We are offering the following service
Medical Billing & Claims Processing
- Charge Entry: Accurate entry of patient and provider details into the billing system.
- Claims Submission: Electronic and paper-based claims submission to insurance payers.
- Claim Scrubbing: Pre-submission checks to ensure claims are free from errors.
- Follow-up on Claims: Tracking claim status to ensure timely processing.
- Electronic Remittance Advice (ERA) Posting: Automatic posting of payments received.
- Reconciliation of Payments: Ensuring received payments match expected reimbursements

Medical Coding Services
- ICD-10, CPT, and HCPCS Coding: Accurate assignment of codes for diagnosis and procedures.
- Compliance & Regulatory Updates: Keeping up with the latest coding guidelines and payer policies.
- Coding Audits & Reviews: Ensuring coding accuracy and compliance with payer requirements.
- Specialty-Specific Coding: Tailored coding services for various medical specialties.
- Charge Capture Optimization: Ensuring all services rendered are coded and billed correctly.

Insurance Verification & Authorization
- Eligibility Verification: Checking patient insurance coverage and benefits.
- Prior Authorization Requests: Submitting authorization requests for necessary procedures.
- Coordination with Payers: Communicating with insurance companies for approvals.
- Updating Patient Records: Documenting verified insurance details in the system.
- Real-time Insurance Checks: Utilizing electronic verification systems for quick results.

Denial Management & Appeals
- Denial Analysis: Identifying common reasons for claim denials.
- Appeal Preparation & Submission: Drafting and submitting appeals for denied claims.
- Corrective Action Implementation: Addressing recurring issues to prevent future denials.
- Payer Communication: Engaging with insurance companies to resolve disputes.
- Monitoring & Reporting: Tracking denial trends and improving claim acceptance rates.

Accounts Receivable (A/R) Management
- Aging Report Analysis: Reviewing outstanding claims and payments.
- Follow-up on Outstanding Claims: Regular follow-ups with payers for unpaid claims.
- Patient Payment Follow-ups: Contacting patients for outstanding balances.
- A/R Cleanup & Recovery: Identifying and resolving backlogged or aged claims.

Patient Billing & Support
- Statement Generation & Mailing: Sending clear and concise billing statements to patients.
- Payment Processing & Reconciliation: Managing patient payments and updating records.
- Patient Support & Query Handling: Assisting patients with billing inquiries.
- Payment Plans & Collections: Setting up instalment plans for patients with financial difficulties.
- Online Payment Portals: Enabling convenient digital payment options.

Credentialing & Provider Enrollment
- Provider Credentialing: Verifying and maintaining provider credentials.
- Enrollment with Insurance Payers: Assisting providers in enrolling with insurance networks.
- Re-Credentialing Services: Managing periodic re-credentialing requirements.
- CAQH Profile Management: Ensuring accurate provider profiles on CAQH.
- Contract Negotiation Support: Assisting in negotiating contracts with payers.

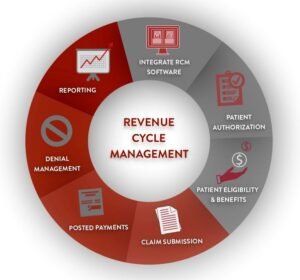
Revenue Cycle Management (RCM)
- End-to-End RCM Services: Managing the entire revenue cycle from patient registration to payment.
- Workflow Optimization: Implementing efficient processes to improve cash flow.
- Financial Reporting & Analytics: Generating reports for revenue insights.
- Compliance & Regulatory Adherence: Ensuring adherence to healthcare regulations.
- Technology Integration: Utilizing RCM software for streamlined billing and collections.